As a practicing veterinarian specializing in small animal medicine, few conditions cause as much discomfort and distress to pets as an anal gland rupture. In both dogs and cats, the anal glands (also known as anal sacs) serve unique scent-marking functions—but when blocked, infected, or inflamed, they can lead to serious complications, including painful abscesses and ruptures.
This comprehensive 2025 guideline provides updated insights into the diagnosis, treatment, and prevention of anal gland rupture in dogs and cats, based on the latest studies in veterinary clinical practice and emerging trends in preventive care.
What Are Anal Glands?
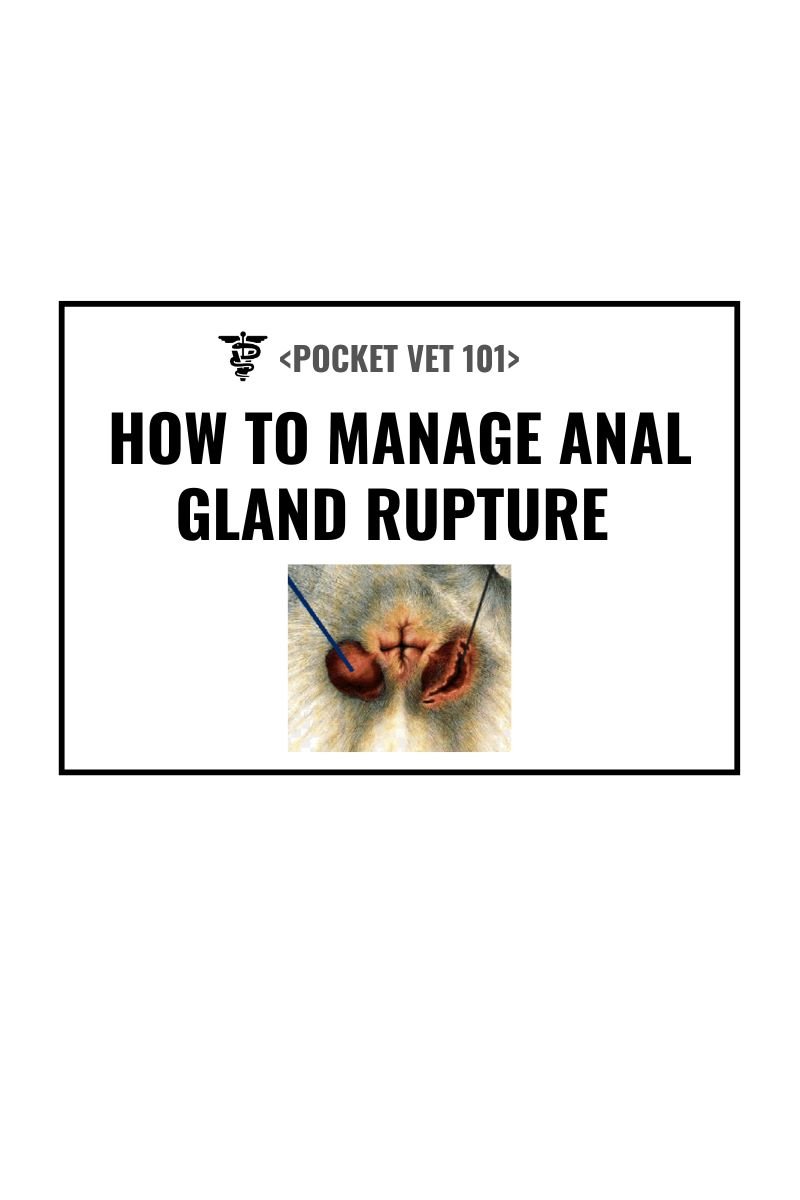
Anal glands are small sacs located on either side of the anus—typically at the four and eight o’clock positions. They contain sebaceous and apocrine glands that secrete a strong-smelling fluid used for communication among animals. Normally, these glands empty naturally during defecation or stress.
However, when the ducts become obstructed or infected, the fluid can accumulate, thicken, and form an abscess. If untreated, pressure within the gland increases until the abscess ruptures through the skin, releasing pus and blood—an extremely painful process for the animal.
Understanding Anal Gland Rupture
An anal gland rupture is the end stage of severe anal sac infection or impaction. What usually begins as mild discomfort rapidly progresses to swelling, abscess formation, and eventual bursting of the gland through the surrounding skin.
Key Symptoms Include:
- Sudden pain near the anus
- Swelling, redness, or open wound beside the rectum
- Blood or pus discharge
- Excessive licking or scooting on the floor
- Crying or biting when tail or hindquarters are touched
- Foul odor from the anal region
In cats, clinical signs may be subtler—such as hiding, decreased grooming, or refusing to sit normally.
Without timely veterinary intervention, secondary bacterial infection and tissue damage can extend deeper, potentially requiring surgical repair or drainage.
Causes and Risk Factors
Anal gland rupture typically develops from one of the following underlying problems:
1. Gland Impaction
When the anal glands fail to empty normally, secretions become thick and dry, blocking the ducts. Obesity, low-fiber diets, or reduced defecation pressure contribute to this.
2. Bacterial Infection (Anal Sacculitis)
Bacteria such as E. coli, Proteus mirabilis, or Enterococcus often infect retained gland secretions, leading to swelling, pain, and eventual abscess formation.
3. Chronic Anal Sac Disease
Recurrent impactions and infections weaken gland tissue, predisposing the animal to rupture.
4. Dietary and Lifestyle Factors
Low-fiber diets, sedentary lifestyles, and chronic soft stools reduce the natural expression of glands during defecation.
5. Breed Predispositions
Small and medium breeds (e.g., French Bulldogs, Cocker Spaniels, Dachshunds) are more prone in dogs; in cats, long-haired breeds (like Persians) may have higher incidence rates due to grooming and hygiene issues.
6. Allergic Dermatitis
Dogs and cats with food or environmental allergies often suffer from chronic anal gland inflammation secondary to skin irritation and over-secretion.
Diagnosis (2025 Veterinary Protocols)
Accurate diagnosis is essential to distinguish anal gland rupture from other perianal conditions such as tumors, fistulas, or trauma.
1. Physical Examination:
A veterinarian performs palpation of the anal glands—usually under light sedation if rupture pain is severe. Visible swelling, ulceration, and drainage are strong diagnostic indicators.
2. Cytology and Culture:
Swabs from the ruptured gland are examined under the microscope and cultured to identify bacterial pathogens and guide antibiotic selection.
3. Imaging (when warranted):
In chronic or complicated cases, ultrasound or contrast radiography helps assess sinus tracts, tissue destruction, or deeper abscesses.
4. Differential Diagnosis:
Conditions such as perianal fistulas, mast cell tumors, or trauma-related abscesses must be ruled out, especially in older or recurrent cases.
Treatment for Anal Gland Rupture
Immediate and thorough veterinary care is necessary to manage pain, infection, and tissue healing. Treatment in 2025 follows a multimodal approach for both dogs and cats, tailored to each patient’s condition.
1. Wound Management and Drainage
- Manual Drainage & Cleaning: Any abscess cavity or ruptured gland is gently flushed with antiseptic solutions (e.g., chlorhexidine or diluted iodine).
- Lancing and Debridement: If abscesses are not self-ruptured, they are surgically opened to allow proper drainage and reduce pressure.
- Warm Compresses: Promote circulation and help the wound heal faster.
2. Antibiotic Therapy
Systemic broad-spectrum antibiotics are initiated based on culture results. Common therapies include amoxicillin-clavulanate, enrofloxacin, or cefpodoxime, continued for 10–14 days.
3. Anti-Inflammatory and Pain Management
NSAIDs (e.g., carprofen or meloxicam) or other analgesics help reduce swelling and pain. Severe cases may require short-term opioids under veterinary supervision.
4. Topical Medications
Antibacterial ointments or medicated wipes may be applied to the surrounding skin to prevent secondary infection.
5. E-Collar (Elizabethan Collar)
Prevents the pet from licking or biting the affected area during recovery.
6. Surgical Intervention (Anal Sacculectomy)
Chronic or recurring infections, especially after repeated ruptures, may necessitate surgical removal of the anal glands. This procedure, known as anal sacculectomy, is often curative when performed by board-certified surgeons using new minimally invasive methods available in 2025 that reduce recovery time and postoperative complications.
Recovery and Prognosis
Most pets begin showing improvement within several days of treatment, with full recovery in 10–14 days if the rupture is uncomplicated.
However, if tissue necrosis, deep infection, or chronic scarring develops, healing may take longer and require additional therapy.
Owners should monitor for recurrence and ensure the glands are functioning properly during future bowel movements. Regular follow-ups are key.
Prevention: 2025 Best Practices
The best way to handle anal gland rupture is to prevent the underlying causes through appropriate diet, hygiene, and monitoring routines.
1. Maintain a Balanced, High-Fiber Diet
A diet rich in fiber (either natural or veterinary-supplemented) helps form firm stools that naturally express the glands during defecation. This is one of the simplest, most effective forms of prevention.
2. Routine Gland Expression
For dogs prone to impaction or small breeds, schedule regular anal gland expression either by a groomer or veterinary technician. Cats seldom require manual expression unless chronic disease is suspected.
3. Weight Management
Obese animals often have underactive gland expression due to reduced muscle tone and defecation pressure. Maintaining an ideal body weight supports anal health.
4. Address Allergies Early
Dogs and cats with recurrent anal gland disease frequently have underlying allergies. Managing skin and food allergies through dietary modifications and anti-allergy medications greatly reduces recurrence risk.
5. Monitor Stool Quality
Any persistent soft stool or diarrhea can contribute to incomplete gland emptying. If noticed, dietary adjustments or probiotic supplementation may help maintain optimal gut health.
6. Hygiene and Grooming
Regular grooming around the anal area prevents fur matting and bacterial buildup—especially important in long-haired cats and dogs.
When to See a Veterinarian
Seek immediate veterinary assistance if you notice any of the following signs:
- Pus or blood near the anus
- Constant scooting or tail-biting
- Sudden swelling, redness, or open wound next to the rectum
- Reluctance to sit, defecate, or walk normally
- Recurrent anal gland infections despite prior treatment
Early detection and professional management can prevent progression to rupture, which is both painful and more complex to treat.
Final Thoughts
Anal gland rupture in dogs and cats may look alarming, but with proper diagnosis, prompt treatment, and consistent preventive care, full recovery is very achievable.